Tales Of Medical Care Struggles Of The Ouaka People In Central African Republic

“We didn’t think Aboubakar would survive,” says Clara, nine-year-old Aboubakar’s aunt, as she recalls how the little boy arrived at the hospital with cerebral malaria. He was unconscious, convulsing, with his tongue hanging out of his mouth.
Aboubakar was admitted to the intensive care unit and seven days later was transferred to the paediatrics unit. Little did Clara know that Aboubakar would be back on his feet just weeks later.
More than 60 km separate Aboubakar’s village of Gotcheke from Bambari regional hospital in Ouaka prefecture, Central African Republic (CAR), which is supported by Médecins Sans Frontières/Doctors Without Borders (MSF).
Clara thought her nephew had died as the family travelled along the bumpy road to the hospital crowded onto the back of a motorbike.
“We have no healthcare in the village,” says Lidi, Aboubakar’s mother. “There’s only a building, with no doctors and no medicine. I couldn’t get a consultation for my child or for myself.”
Lidi speaks with a tone of barely concealed pain. In the past, she had three miscarriages and lost two of her children. One disappeared in the forest and the other died after a sudden and brief illness.
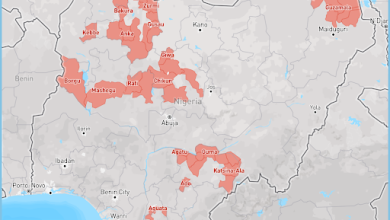
The medical needs and daily struggles of the people of Ouaka are almost invisible to the international community and CAR remains a protracted ‘forgotten’ crisis. The situation in Ouaka reflects similar situations in other prefectures across the country.
Communities in CAR face many persistent obstacles that prevent them from reaching medical care in time. The most serious barriers are displacement from their homes caused by the repeated cycles of violence, and the fact that, for most people, quality healthcare remains unaffordable and unavailable.
The few health facilities that function are ill-equipped, have severe shortages of skilled medical professionals and supplies or are simply out of people’s reach.
Long distances and a deadly journey
The limited number of functioning health facilities drives many people, including Aboubakar’s mother, to find desperate solutions to get hold of medical care.
Lidi had two options if she became pregnant or her children fell ill and needed to reach a health facility: either a seven-km walk through the dense forest, or a costly 25-km motorbike ride along a poorly maintained road, which is almost impassable during the rainy season.
“Some patients have to walk very long distances from their homes to reach a medical facility,” says Roxanne Hagan, MSF’s nursing activity manager in Bambari hospital.
“We had a family that walked an entire day to reach an MSF health post, to then be driven by an MSF vehicle to the hospital. Many patients arrive in a late stage of their illness; one of the main reasons is the distance and time it takes to arrive at the health facility.
“We receive patients who are severely-ill because treatment was delayed. Sometimes, they are so ill that there is little chance we can save them,” Hagan added.
Twenty-year-old Aïssatou has given birth to three children. One died at the age of six as they travelled by motorbike to reach a hospital for medical treatment.
Now she is in the hospital with her daughter Ryana, aged nine months, who she brought to the hospital with breathing problems. When the doctors examined her, they discovered she had cardiomegaly; an abnormal enlargement of the heart that is untreatable with the resources available in CAR.
After more than seven weeks in the hospital, the MSF team has treated all the secondary diseases caused by Ryana’s heart problem. Unable to breathe independently, she relies on a supply of bottled oxygen to keep her alive.
In mid-2018, widespread insecurity forced the MSF-supported health centre in the Élevage neighbourhood of Bambari to suspend its activities for over a week. The closure took its toll on people who relied on the centre’s healthcare services.
The insecurity and fear of violence also meant fewer people were willing to travel to a hospital, even if they needed urgent medical care. As a result, the MSF-supported Bambari hospital saw a decline in medical activities, while those patients who arrived were often in a critical condition.
Sixty-year-old Hamad, Bambari Mosque’s third Imam, is still traumatised by the events he lived through in 2018. He recalls how he was sitting in front of his house when a military operation started nearby. His foot was injured by a stray bullet, which left a mark that is still visible two years later.
While Ouaka has seen a decline in the levels of violence over the past two years, indiscriminate attacks and intermittent fighting – worsened by the presence of armed groups – occur regularly.
On December 7, just a day after Hamad shared his painful memory, Bambari was again overrun by violence.
The striking levels of violence in an and around the city have had a serious impact on people’s lives, particularly their access to essential healthcare. Nineteen-year-old Marie was experiencing convulsions in the operating room of Bambari hospital as she waited to give birth by emergency caesarean when the shooting erupted in Bambari.
The gunfire and mortar exchange lasted for hours and suspended much of the city’s activities. Marie’s family were able to shelter inside the hospital, but there was a much bigger problem.
“Because of the shooting, the medical staff were not present in the hospital,” says Marie’s mother. “They’d fled home for safety or hadn’t come to work that day. I was worried and stressed, but there wasn’t much I could do. I didn’t close my eyes that entire night while my daughter was convulsing.”
After waiting long hours until daylight, the medical team arrived at the hospital and came to Marie’s rescue. Later that morning, she underwent the caesarean, which was complex to carry out due to the convulsions. But both she and the baby were fine. She regained consciousness to find her family all around and her boyfriend at her side.
Financial barriers to healthcare
“I don’t have the means to take care of my health,” says Christine, who has been living in Ngakobo camp for displaced people since 2018.
There are currently close to 192,000 displaced people living in displacement sites and an estimated 440,000 living in host communities across CAR, not to mention a large number of refugees in neighbouring countries.
The displaced people left their homes to flee violence and are now living in precarious situations, which makes them among the most vulnerable people in the country. “I feel useless,” she says. “If my husband had the money, I could go to Bambari hospital.”
Christine is blind and has fallen ill a number of times since she fled her home, which never happened to her before. Punctuated by heavy fits of coughing, she explains how she got the medicine from her community to treat her cough, but the medicines did not get rid of it, and she cannot afford to buy more.
Awa’s situation is similar in that she faces financial constraints which have put medical care out of reach.
She is relieved that her son, Bilal, who is malnourished, receives free-of-charge treatment at Bambari hospital; however, she cannot afford medical care for herself. Her family lost all their livestock during the conflict and are now forced to live off the little money her husband makes from collecting and selling wood.
Since she fled, she has always been sick, with a sore throat and sores in her mouth; sometimes she even vomits blood. Without the money to pay for a consultation and medication, her health problems remain uncared for.
The use of traditional medicine is a widespread practice followed by many people in CAR who cannot afford conventional medical treatment. “Consultation with a traditional practitioner is the first step for many patients,” says Adelaïde Ouabo, MSF medical coordinator.
“Due to the distance and the high cost of transport to reach the hospital, patients resort to traditional practitioners. Such practices, if not administered by a trained medical professional, could prove harmful to their health,” Ouabo added.
Mariam, aged 35, gave birth to all her children at home. Her eldest child was treated by a traditional practitioner for swellings to his body. “We don’t have the means for treatment at the hospital, not even the strength to work or earn enough to eat,” she says.
MSF has been working in Bambari hospital since 2014 where its teams manage the inpatient therapeutic feeding centre, the neonatal unit, the paediatric ward, the surgical ward and treatment for survivors of sexual violence.
Since the beginning of 2020, MSF teams have provided 70,000 consultations and admitted 3,600 people as inpatient. In the areas around Bambari, MSF is also supporting three health centres and seven antimalaria hubs.
MSF has worked in CAR since 1997 and currently runs 14 medical programmes in Bangui, Bambari, Bangassou, Batangafo, Bria, Bossangoa/Boguila, Carnot, Kabo, Paoua and Zemio.
Support Our Journalism
There are millions of ordinary people affected by conflict in Africa whose stories are missing in the mainstream media. HumAngle is determined to tell those challenging and under-reported stories, hoping that the people impacted by these conflicts will find the safety and security they deserve.
To ensure that we continue to provide public service coverage, we have a small favour to ask you. We want you to be part of our journalistic endeavour by contributing a token to us.
Your donation will further promote a robust, free, and independent media.
Donate HereStay Closer To The Stories That Matter