World Diabetes Day: A Diabetic Patient in Rural Nigeria Shares His Battle for Survival
From inadequate knowledge and lack of care to poor access to standard healthcare, HumAngle sheds light on the plight of diabetic patients in rural northeastern Nigeria as the world marks World Diabetes Day with the theme, ‘Breaking Barriers, Bridging Gaps.’

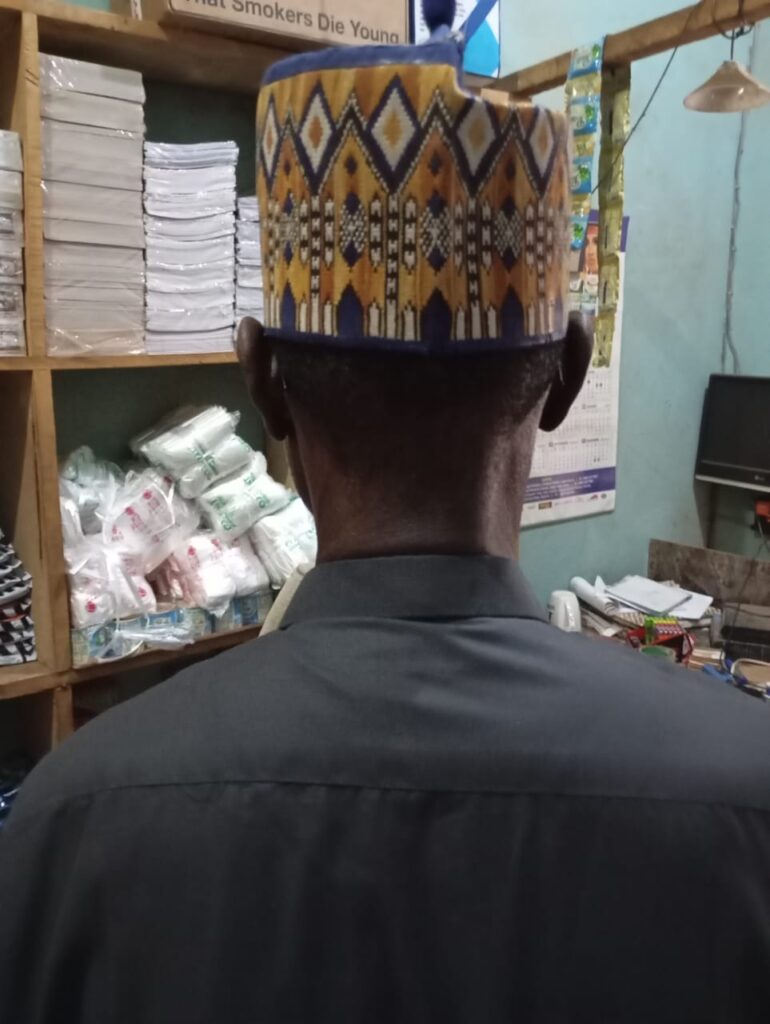
For over three decades, Ahmed Abubakar, a 67-year-old trader from a small community in Potiskum, Yobe State, northeastern Nigeria, has lived with diabetes.
“I was diagnosed in 1990,” he told HumAngle.
At the time, Ahmed worked as a labourer and initially attributed his persistent thirst to the nature of his work. “I would drink water and then feel thirsty almost immediately,” he recounted. Ahmed also noticed frequent trips to the restroom, an early sign of his condition.
Ahmed’s life changed drastically following his diagnosis. He had to quit his job, as manual labour demands were too much for his condition.
“I was also told to stop eating certain foods, but then I’d go home and find the usual meals prepared. I had no choice but to eat it,” he explained. Over time, his body began to ache intensely, sometimes feeling as if he had been severely beaten.
World Diabetes Day, observed on Nov. 14 annually, aims to “raise awareness about diabetes as a critical global public health issue and emphasise the collective and individual actions needed to improve the prevention, diagnosis and management of the condition.” This year’s theme, ‘Breaking barriers, bridging gaps,’ underscores the risk of diabetes and the need for comprehensive, affordable treatment for everyone affected.
Diabetes is a chronic condition characterised by the body’s inability to produce or effectively use insulin, a hormone that regulates blood glucose levels.
Dr Isaac Dika, a medical doctor at the Modibbo Adama University Teaching Hospital, Yola, told HumAngle that diabetes cases are rising in Nigeria.
“Some people just sit at home and eat junk food,” he said. “They don’t get involved in exercise or physical activities, which has increased the prevalence of this disease. Everybody is either on soda or energy drinks; these high-calorie intake diets predispose individuals to diabetes, while for others, it can be hereditary. Their parents have diabetes, so they are likely to have diabetes due to genes.”
Additionally, Dr Dika noted that apart from people with a family history of diabetes, those with high blood pressure and those who are obese are more susceptible. “There are also certain medications like antipsychotics and long-term steroids that tend to predispose people to diabetes,” he added.
The International Diabetes Foundation reports that 3.6 million cases of diabetes have been recorded in Nigeria, with a 3.7% prevalence in adults. Typical disease symptoms include excessive thirst, hunger, frequent urination, slow-healing wounds, and tingling sensations in the hands and feet.
The diabetes crisis in rural Nigeria
Ahmed’s journey with diabetes is a difficult one, as he described it. At a point, his family had to compromise and cook his meals separately when his health began to deteriorate.
“I stopped eating rice, bread, certain grains, and tea, among others,” he said, noting that certain fruits like orange and pineapple were scrapped out of his diet. A change he was not happy with but had to accept for the sake of longevity.
Globally, the World Health Organisation (WHO) estimates that 422 million people live with diabetes, with 1.5 million deaths recorded annually. Most cases are in low- and middle-income countries.
According to Dr. Dika, managing diabetes is often cost-prohibitive. “One of the reasons why people of low socio-economic status tend to develop diabetes the most is due to poor health-seeking behaviour,” he said. “Their diet is usually carbohydrate-based, and since they have poor health-seeking behaviour, they hardly go to the hospital and don’t go early when diabetes sets in.”
Dr. Isaac further explained that late diagnosis coupled with poor management can lead to diabetic neuropathy, a type of nerve damage that can occur if you have diabetes; it affects mainly the feet and hands. In other cases, it can lead to kidney problems and diabetic retinopathy, which has to do with issues with sight leading to subsequent blindness. Other complications include hypertension and stroke.
“One of the key things I think government health systems can do is to make testing free, especially for adults who are more at risk of diabetes type 2. This can lead to early detection and prompt management of the disease.” Dr Dika suggested, stressing the need for government-subsidised medication for diabetes patients.
Ahmed has managed to follow his diet and medication thanks to his family and a consultant who occasionally visits his community to check on diabetic patients. However, this support is inconsistent. “Sometimes he comes after three months, and I go to him when he comes,” he said.
However, he has to rely on local healthcare providers in his community who lack specialised knowledge during emergencies. He recounted that “there was a time I was restless, and the drug the local health care workers gave me didn’t work. I had to travel to Azare in Bauchi to see another consultant who tended to me.”
Aside from inflation driving up food prices, Ahmed’s biggest concern is his deteriorating eyesight—a common complication of diabetes. “Sometimes, I can’t see people from a distance, and it’s worsening. The consultant said it’s because of the diabetes,” he explained, adding that he’s also been suffering from severe stomach pains.
Despite his dedication to his diet and medication, Ahmed’s medication supply is inconsistent, often leaving him anxious about when he’ll next see the consultant or afford his prescriptions.
The mental toll of living with diabetes
Research from the International Diabetes Federation shows that 75 per cent of people with diabetes desire emotional and mental support from their healthcare providers, with many suffering from anxiety or depression.
Ahmed acknowledges that there are days when his condition overwhelms him. “Sometimes, it’s as if the pills are not working, but I keep taking them anyway,” he said. “There was even a time when I was bedridden for nine days. I couldn’t eat properly or drink water. I kept feeling weak and nauseous until I got better.”
More barriers and the way out
According to Dr Dika, insulin and other diabetes medications require proper storage, which rural health centres often lack. “The government should also invest in local pharmaceutical companies so that they can produce these drugs that we need locally and so that the cost of production won’t reflect on the medication,” he said.
“We have a healthcare problem in this community, and I can tell you that there are a lot of people living with diabetes but don’t have the means to manage it. I hope the government can support locals here not necessarily with money but with medication because these drugs are quite expensive, as well as our diet,” according to Ahmed.
Dr Dika echoed this sentiment, calling for a healthcare strategy prioritising diabetic patients’ needs. He advises regular exercise, reduced intake of carbohydrates, a balanced diet incorporating fruits and vegetables, and limiting alcohol intake.
He further suggests that the government provide free diabetes screenings, especially for adults over 45, for early detection and prompt management. “Routine glucose testing, including fasting and random blood sugar tests, should be standard practice,” he noted.
Like many other diabetic patients, Ahmed is uncertain about his future, living each day with the hope that his efforts are enough to manage his condition.
Additional reporting by Aisha Umar Gimba
Ahmed Abubakar, a trader from northeastern Nigeria, has managed diabetes for over 30 years, though his journey is filled with challenges due to poor access to healthcare and proper knowledge.
On World Diabetes Day, the plight of diabetic patients in rural areas highlights the urgent need for better healthcare access, affordable medications, and healthy dietary options. Dr.
Isaac Dika emphasizes the rising diabetes cases influenced by sedentary lifestyles and high-calorie diets, noting limited healthcare resources in rural areas, complicating disease management.
Diabetes management often proves cost-prohibitive, particularly for those with limited means, as Ahmed illustrates with his struggle for medication consistency and adequate medical support.
The lack of specialized healthcare in his community leaves him dependent on infrequent medical visits, exacerbated by issues like deteriorating eyesight and potential diabetic complications. Dr. Dika advocates for government intervention to ensure free testing, local drug production, and comprehensive diabetic care, calling for proactive health strategies.
Emotional difficulties accompany these physical challenges, with many diabetic patients facing mental health pressures, underscoring the need for complete support systems.
Support Our Journalism
There are millions of ordinary people affected by conflict in Africa whose stories are missing in the mainstream media. HumAngle is determined to tell those challenging and under-reported stories, hoping that the people impacted by these conflicts will find the safety and security they deserve.
To ensure that we continue to provide public service coverage, we have a small favour to ask you. We want you to be part of our journalistic endeavour by contributing a token to us.
Your donation will further promote a robust, free, and independent media.
Donate HereStay Closer To The Stories That Matter




